Dysphonia is an impairment of the voice and can be caused by various or multiple factors including laryngeal trauma, vocal overuse, medications, reflux, allergies or post-nasal drip, or reduced breath support. Some symptoms include a voice that sounds hoarse, raspy, breathy, or strained, and sometimes can also break or change in pitch. Dysphonia can cause difficulty in communication and can restrict everyday activities. Therapy usually includes learning about vocal hygiene, improving breath support, and strategies for healthier vocal habits to improve the voice and reduce the risk of recurrence.
Vocal Hygiene
Here are general strategies to improve vocal hygiene:
- Stay hydrated. Dehydration can increase the risk of vocal fold irritation, increase the viscosity of vocal folds, reduce vocal fold mobility, and increase the effort required for speech.
- Avoid Caffeine and alcohol. They can dehydrate the vocal folds, so try to avoid these or at least make sure you are also drinking water to avoid dehydration.
- Avoid yelling or shouting. When possible, avoid talking in noisy environments and turn off the TV when talking to avoid having to raise your voice.
- Try to reduce the distance between you and the person you are speaking to. This is more difficult during COVID, but when you are with family try to be within 3 feet of your conversation partner so you will not have to raise your voice to be heard.
- Limit the amount of time talking if possible. Rest your voice after a long day of talking or take breaks throughout your day.
- Avoid airborne irritants like cigarette smoke.
- If you are prescribed a reflux or allergy medication, take it as prescribed. Reflux or post-nasal drip can irritate the vocal cords and taking your prescribed medication will help reduce that risk.
- Reduce throat clearing or coughing. If your throat feels irritated, try a sip of water or a hard swallow instead.
- Warm up your voice before singing. A speech pathologist can give you appropriate vocal exercises.
- Try to breathe through your nose instead of your mouth to reduce drying your vocal folds. If the air is dry, consider a humidifier.
Breath Support
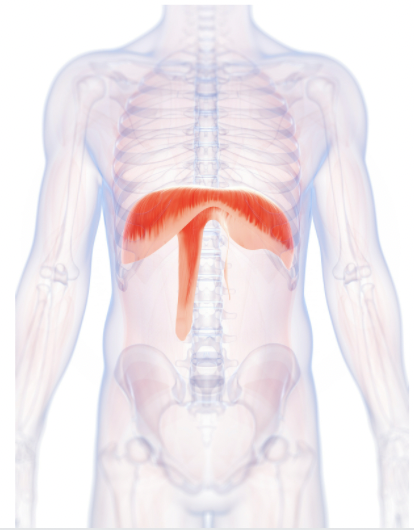
Adequate breath support is crucial for good vocal hygiene and habits. Voice is produced through your exhale and the vibration of your vocal folds. Adequate breath support helps reduce excess tension which can strain the vocal folds.
Diaphragmatic breathing is the most efficient and natural breathing pattern. The diaphragm is a large, dome-shaped muscle that separates your chest cavity (where your heart and lungs are) from your abdominal cavity (where your digestive organs are). When you inhale, the diaphragm contracts and moves downward, increasing the size of your chest cavity and allowing the lungs to expand. When you exhale, the diaphragm relaxes and rises and your chest cavity reduces in size. When using diaphragmatic breathing, it is important to reduce any tension in the use of muscles around the neck. When asked to take a big breath, many voice clients tend to use muscles near their neck, but this can cause excess strain on the vocal system. Instead, keep muscles around your neck and shoulders relaxed while focusing on using your diaphragm. Using your diaphragm will help increase your capacity to speak longer and with reduced strain.
Here is how you can start practicing diaphragmatic breathing at home:
- Sit up straight or lay down. Most patients find it easier to start out laying down because more of your muscles can relax rather than having to hold yourself up.
- Place one hand on your chest and the other on your stomach.
- Take a slow, deep breath through your nose. As you inhale, you should feel the hand on your stomach, not your chest, moving outward as your diaphragm contracts and allows your lungs to expand.
- Breathe out through pursed lips completely emptying your lungs. You should feel the hand on your stomach moving inward.
- Your goal is to complete 6 – 10 slow breaths per minute without holding your breath between breaths.
- If at any point you feel dizzy, take a break and return to your normal breathing pattern.
Voice Therapy
If you are having difficulty with your voice, ask your doctor to refer you to a speech therapist for an evaluation and treatment. It may also be helpful to get a referral to an ear, nose and throat doctor (or ENT) to further evaluate. Therapy involves various vocal exercises and gradually increasing the difficulty by starting at the single syllable or word level and later implementing the techniques in conversation. The goal of these vocal exercises is usually to improve resonance and airflow, and reduce vocal strain. Your therapist will help you find exercises that work best for you and recommend a home exercise program to complete daily.
0 Comments